Laser correction of myopia, hyperopia and astigmatism FEMTOSECOND LASIK and PRK
FEMTOSECOND LASIK KAI PRK
Do you wear glasses or contact lenses? Are you dependent on them but don’t want to wear them anymore? Have you ever thought what your life would be like without your glasses? Now you can!!
Rapid developments in biomedical technology and ophthalmology allow us today to correct myopia, hypermetropia and astigmatism with a laser and get rid of our glasses and contact lenses. The results are spectacular. The operation is performed quickly, painlessly and the patient leaves the operating room after a short while without bandages.
What are refractive errors?
Refractive errors or ametropia are myopia, hypermetropia, astigmatism and presbyopia.
Myopia occurs either because the anterior surface of the eye (the cornea) is very convex, or because the eyeball is large in size, or both. The image forms in front of the retina of the eye. Vision for distant objects is blurred.
In hyperopia the eyeball is usually smaller. The image forms behind the retina (at the back) of the eye. Vision is blurred for both near and distant objects.
With astigmatism, the curvature of the cornea is not regular with the result that the image appears blurred.
Presbyopia is considered a normal ageing process of the eye, which occurs after the age of 40 and is due to the gradual loss of the len’s ability to adapt to focus on near objects. As a result, near vision is not very good and corrective glasses are needed.
How are refractive errors treated?
The classic way to deal with refractive errors is with glasses and contact lenses. For various reasons, many people do not want to wear them, either because they are tired after using them for years or for aesthetic or professional reasons or because they cannot tolerate contact lenses (intolerance, allergies, giant papillary conjunctivitis ). For these people laser correction is indicated.
Refractive surgery includes all those techniques that allow us to correct some ametropia. It is carried out by ophthalmologists who specialize in this field. It corresponds to plastic and cosmetic surgery since we change our cornea and it is often done for aesthetic reasons. Lasers play a very large role in ophthalmology and refractive surgery. The experience is not new in ophthalmology. We now have nearly 30 years of experience, while the evolution of laser technology now allows us to have much better functional and predictable results.
 Who can undergo this surgery?
Who can undergo this surgery?
Theoretically, any person who has a refractive error can undergo laser correction surgery if they consult an ophthalmologist and there are indications. The following may be eligible candidates:
- Anyone who, for any reason, doesn’t want to or can’t wear glasses (pilots, athletes, firefighters, police etc.) or who has a problem with their contact lenses.
- Anyone who is over 18 years old and whose refraction has remained stable over the previous year.
- Generally, anyone who is concerned with their appearance and who wants to have good quality vision without being dependent on glasses or contact lenses.
How does laser correction work?
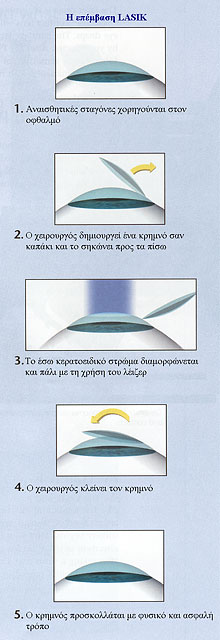
The type of laser used for these cases (excimer laser) works by shaping the surface of the cornea to eliminate or reduce the abnormality. The technique that is most commonly performed today all over the world is the Laser In Situ Keratomileusis (LASIK) which is a combination of microsurgery and laser.
LASIK is suitable for myopia from -1.00 to -10.00 D and depending on the indications. Hyperopia and astigmatism have more limitations (up to 6 degrees), however it can be used to reduce the abnormality if it is greater.
The surgeon creates, with the help of a microkeratome, a flap in the cornea like a cap and lifts it backwards. Nowadays, the flap is created with the help of another laser, FEMTOSECOND LASER, and the technique is called FEMTOSECOND LASIK. Then the second laser, the excimer laser sculpts the surface of the corneal layer without injuring it. The flap is closed and that’s the end of the operation. The operation is done with drops and is completely painless. The application of the laser takes less than 1 minute while the whole process takes no more than 5-10 minutes. No protective lens or sutures are needed and there is no pain or discomfort postoperatively. In this way, the immediate restoration of vision (within a few hours) is achieved and the possibility of some postoperative haze of the cornea is minimized. The patient leaves the operating room without bandages and without the need for glasses.
Results
With the laser the results are very impressive and the purpose is to take away the patient’s need for glasses and contact lenses. Achieving a plus/minus 0.50 of a degree is considered a success and we can achieve this in almost 99% of cases. Technology has made such significant leaps that today we consider this operation to be completely successful, reliable and very safe. Technology allows us to know preoperatively if the patient is a good candidate for surgery and if we can proceed safely. Not everyone can undergo this correction as there are contraindications but we are able to know this before the operation and inform our patient about the possible result.
Preoperative examinations - Technology
 Prior to laser correction, some preoperative ophthalmological examinations and measurements should be performed. These tests and measurements are very important as the result depends directly on the consistency and accuracy with which we make these measurements. It is important to know that in order to get accurate results, contact lenses should not be worn for at least 10 days before the examinations and the operation.
Prior to laser correction, some preoperative ophthalmological examinations and measurements should be performed. These tests and measurements are very important as the result depends directly on the consistency and accuracy with which we make these measurements. It is important to know that in order to get accurate results, contact lenses should not be worn for at least 10 days before the examinations and the operation.
It is therefore necessary to measure with great accuracy the myopia or hypermetropia or astigmatism without, but then with drops that open the pupil.
 A corneal topography (ORBSCAN, PENTACAM) should be performed, which allows us to assess and measure its surface, to rule out diseases that are contraindications for surgery (eg keratoconus) as well as to estimate its thickness. The thickness measurement is a very important measurement which dictates how much we can sculpt with the laser. If there is not enough tissue then the operation can not be done.
A corneal topography (ORBSCAN, PENTACAM) should be performed, which allows us to assess and measure its surface, to rule out diseases that are contraindications for surgery (eg keratoconus) as well as to estimate its thickness. The thickness measurement is a very important measurement which dictates how much we can sculpt with the laser. If there is not enough tissue then the operation can not be done.
The laser used by the doctor is the latest generation ALCON WAVELIGHT LASER SUITE
Alternative laser correction techniques
One of the alternatives for laser myopia correction is the PRK technique (photorefractive keratectomy). In PRK no flap is created, the corneal epithelium is simply removed and the laser is applied directly. A variation of this technique is trans PRK where the epithelium is not removed at all. At the end of the operation, a therapeutic contact lens is applied until the epithelium heals. This technique can be applied when the thickness of the cornea does not allow us to make use of lasik.
What happens with major refractive errors?
Fifteen years of experience with lasers has shown that with greater ametropias, myopia above 10-11 degrees and hyperopia above 4-5 degrees, we have better results by resorting to conventional surgery or a combination of conventional and laser surgery. This is because the thinning of the cornea is beyond some permissible limits in very large degrees of myopia and hypermetropia putting the safety of the eye at risk.
Very high ametropias are best treated with surgery that involves the insertion of permanent intraocular lenses (lenses that are placed inside the eye). There are special intraocular contact lenses that are placed either behind the iris (ICL) or in front of the iris (ARTISAN). The advantage of this method is that it is reversible. That is, the lens can be removed if there is a reason to, something that is not achievable with laser surgery. For better and more predictable results, these techniques are combined with the laser (bioptics), which is performed shortly after the intraocular lens is inserted and we have a finalised visual acuity. The laser is used to achieve the desired results, correcting the rest of the ametropia that is probably still present after the insertion of the lens.
If there are already some opacities of the natural lens of the eye and if there is a high degree of myopia coupled with an older age, an alternative operation is the refractive lensectomy (clear lens extraction), ie the removal of the lens of the eye in a similar way to how it is removed for a cataract and the insertion of a corrective intraocular lens. Refractive lensectomy is for older people who have very large myopia and, at the same time, a possible future cataract can be removed early.
In large astigmatisms, astigmatic keratotomies can be performed, i.e. small diametrically opposed incisions in the cornea to change its abnormal curvature. In pathological conditions such as keratoconus, in which we have very large astigmatisms, corneal transplantation is indicated.
Complications
Refractive surgery is one of the safest surgeries performed on the human body. However, every operation hides potential (although rare) risks of complications of which we must be aware.
a) Refractive complications
LASIK can lead either to overcorrection or undercorrection due to the differences between patients in terms of healing and other surgical parameters, leaving patients with myopia, hypermetropia or astigmatism. These may force the patient (or maybe not) to wear glasses, lenses or to undergo additional surgery.
Prevalence of correction: 1 in 100
Prevalence of correction: varies depending on the patient’s prescription eg 4 in 100 for myopia with 4D, 8 in 100 for myopia with 8D.
b) Regression
This refers to the tendency of the eye to partially regress towards the initial degree of the refractive problem following laser correction. In most cases the regression is small and is taken into account when planning your surgery. Often the only thing needed for patients with regression problems is glasses at night.
Prevalence: 1 in 100
c) Loss of best corrected vision
A small number of patients show a small loss in visual acuity after laser correction. This means that after your surgery, even wearing glasses or contact lenses, you may not be able to see as clearly as you did before the operation. In most cases the acuity returns within a period of 6 to 12 months.
Prevalence: 1 in 100
d) Night reflections
Even before undergoing laser correction, many people have poor night vision or nocturnal reflections ("haloes", "star bursts") when wearing glasses or contact lenses.
Nocturnal reflections are common immediately after surgery and usually last 3 to 4 months. Once both eyes have healed or six months after surgery, nighttime reflections tend to diminish and vision should return to normal. However, you may still need glasses when driving at night.
Prevalence of severe nocturnal reflections: 1 in 50
e) Postoperative haze
‘Healing haze’ is the collagenous protein that grows on the surface of the eye after surgery, mainly PRK. It is not visible to the naked eye. Although it is possible to cure it in most cases, it usually clears up gradually within many months after surgery.
Prevalence of severe cases: 1 in 1000
f) Infection
Perhaps the most serious complication. The biggest risk of this is probably in the first 48-72 hours after surgery. You will receive antibiotic drops both before and after surgery to prevent possible infection. Most minor infections are cured and eliminated quickly. Rarely there are corneal infections (keratitis) that can seriously affect the eye and consequently vision.
Prevalence of severe infection: 1 in 10,000
g) Epithelial ingrowth
This occurs when cells of the epithelial surface grow below the corneal flap during the healing of the corneal incision. It usually occurs in the first month and is more likely in a patient with a weak adhesive layer for which age is a parameter. Intraepithelial growth is more common in cases of trauma to or rupture of the epithelium. The condition is more common with LASIK surgery and with long-term contact lens wearers. Although most small areas of epithelial growth require only monitoring, large areas require flap lift and cell cleansing.
Prevalence: 1 in 100
h) Corneal flap complications
The primary advantages of the LASIK method are related to the creation of the protective corneal flap. The corneal flap must be clinically sufficient in quantity, thickness and size to proceed with the laser treatment. The risk of corneal flap complications ranges from cases that simply require postponement of the operation for 3-6 months, to cases that create permanent corneal abnormalities resulting in blurred vision.
Corneal flap complications that occur after LASIK surgery during the recovery period include displacement, flap folds, and epithelial growth. The FEMTOSECOND LASER has increased the safety and greatly reduced the complications in creating the flap.
See the world through new eyes. It is worth the effort.
The doctor’s goal is not to offer as many surgeries as possible but to inform the prospective patients and advise them on whether they are good candidates, including information on the expected result and the existing risks. It is also important to recognize your individuality. Each person will have a different perspective when deciding during the evaluation process for the laser correction. You need to respect the limitations of refractive surgery. Not everyone is a good candidate for surgery, and some people are reluctant to accept that. It is more important to know who is not a candidate for surgery. Restraining your expectations and perceptions is the key to successful refractive surgery. Just how satisfied you will be with the result depends on whether your expectations were met to the desired degree or even to a greater degree.
In terms of cost, this depends on the center and the surgeon. The cost is not prohibitive nowadays. We should look at this surgery as an investment for life since the result does not change over time. Think about how much you spend on your contact lenses and their fluids each year or the cost of a pair of good corrective glasses that need to be replaced every now and then because their lenses wear out or because your frame is out of fashion?
However, before making any move, visit an ophthalmologist and especially one who has experience of such operations.