Glaucoma
An information guide for the modern prevention, diagnosis and treatment of glaucoma
What is glaucoma?
Glaucoma is a group of major eye diseases that affects about 2% of the population. It is a disease that leads to blindness if not diagnosed and treated in time. Prevention, in this case, acquires an extremely important character.
Glaucoma, then, is a serious, chronic progressive disease of the optic nerve and optic fibres of the eye that leads to morphological lesions in the optic nerve and in the visual field.

Photo 1: Normal optic nerve
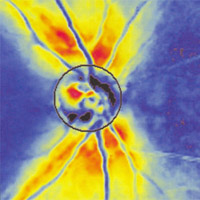
Photo 2: Glaucoma optic nerve
Imagine the optic fibres as many "wires" that join at one point and form a "cable", the optic nerve. In glaucoma, the initial lesions appear in the optic fibres and then transfer to the optic nerve. It is an insidious disease because it has no symptoms (with the exception of some types of glaucoma, such as acute glaucoma) and when the first symptoms appear the lesions are advanced and unfortunately irreversible.
It is a disease for which we can control its progression with the appropriate treatment.
What causes it? Aetiology, pathogenesis.
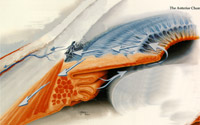 Glaucoma usually occurs after the age of 40. It is more common in people with a family history of glaucoma. It is an inherited disease in about 20% of cases. It also occurs more often in myopics, diabetics and long-term cortisone users. It is due to the imbalance between the production and drainage of a fluid (aqueous humour) that is normally produced inside the eye. This disorder can cause increased intraocular pressure (normal values up to 21 mmHg) which over time can cause damage to the optic nerve. In some types of glaucoma, reduced blood flow may coexist with the result that the optic nerve is not properly nourished. Causes that create reduced blood flow are mainly those related to the cardiovascular system.
Glaucoma usually occurs after the age of 40. It is more common in people with a family history of glaucoma. It is an inherited disease in about 20% of cases. It also occurs more often in myopics, diabetics and long-term cortisone users. It is due to the imbalance between the production and drainage of a fluid (aqueous humour) that is normally produced inside the eye. This disorder can cause increased intraocular pressure (normal values up to 21 mmHg) which over time can cause damage to the optic nerve. In some types of glaucoma, reduced blood flow may coexist with the result that the optic nerve is not properly nourished. Causes that create reduced blood flow are mainly those related to the cardiovascular system.
Pressure in the eye is undoubtedly an important risk factor but it is not enough on its own to make the diagnosis and this is because there must be damage to the optic nerve and optic fibres to be sure of the diagnosis of glaucoma. There are also forms of non-pressure glaucoma (normal or low-pressure glaucoma) in which pressure plays a smaller role.
If there is increased pressure in the eye and there is no damage to the optic nerve, optic fibres and visual field then we are talking about ocular hypertension and not glaucoma. It is a condition that does not necessarily require treatment but close monitoring. In should be noted that only one in ten patients with ocular hypertension eventually develops glaucoma after 5 years. But if the pressure is higher than 28 mmHg, then the chances of developing glaucoma are higher.
THEREFORE INCREASED PRESSURE IN THE EYES DOES NOT ALWAYS MEAN GLAUCOMA.
Types of glaucoma
- Chronic open-angle glaucoma (most common).
- Normal or low pressure glaucoma.
- Closed or narrow angle glaucoma (acute or chronic).
- Secondary glaucoma (after inflammation, trauma, surgery, drugs, etc.).
- Congenital glaucoma (occurs in early childhood).
Diagnosis - monitoring
The developments that have taken place in recent years in medical technology are very important. Technology has given us great potential in both the diagnosis and treatment of glaucoma. Diagnosis is the most important part of studying and monitoring a patient as it will determine whether or not treatment is needed and what type of treatment is appropriate.
 Tonometry
Tonometry
Tonometry is the examination in which the pressure of the eye is measured. It is carried out with both a contact tonometer and an air tonometer.
Gonioscopy
With the help of a special contact lens, the drainage system of the eye (between the iris and the cornea) is examined to know the type of glaucoma and to find any lesions that prevent the drainage of the aqueous humour.
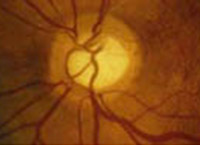 Ophthalmoscopy
Ophthalmoscopy
During this examination and with the help of a special lens, we clinically evaluate the optic nerve. The photo shows a glaucoma optic nerve with a large cavity.
The above examinations can and should be done not only in a specialized glaucoma centre but also in any ophthalmology clinic.
Study of the visual field or perimeter
The study of the visual fields is a very important examination and should always be done when faced with a suspected glaucoma. The patient should recognize bright white spots - targets on a white background.

Photo 1: Automatic perimeter

Photo 2: Glaucoma visual fields
OCT
OCT (Optical Coherence Tomography) is a technology that gives us an image of a tomographic transverse representation of the retina, ie the layers of the fundus (back) of the eye. With this technology we can study and measure the thickness of the optic fibres that are affected early in glaucoma as well as the parameters of the optic nerve.
Corneal thickness
Measuring corneal thickness is considered an important consideration today as thickness can affect the measurement of pressure, i.e. overestimating the pressure with a thick cornea or underestimating it with a thin cornea. Consequently, we can make an incorrect measurement of eye pressure if we do not take into account the thickness of the cornea. The examination is performed with an ultrasonic caliper and only a small contact with the cornea is sufficient or with an optical caliper (ORBSCAN) during corneal topography
Why the need for all this technology?
In glaucoma, the deterioration of the visual field over time is a given if no treatment is received. The patient has no symptoms except when the lesions in the visual field have become very advanced and we are just a few stages before blindness. Then the effects on vision begin to be perceived.
Damage to the field of view begins to be apparent after 30-40% of the optic fibres are lost. The concern of scientists and technology has been focused on the early diagnosis of glaucoma, ie when the visual fields are still normal. All the above technology, which is pioneered by our Centre, helps to make an early diagnosis of glaucoma. Damage to the optic nerve, optic fibres and optical fields, and especially their changes in sequential examinations, are the most important factors in the monitoring of glaucoma over time. The goal is to prevent the progress of glaucoma and to keep the lesions at as early a stage as possible. In this way, vision will not be affected.
How often should we be examined?
The diagnosis of glaucoma is a very important diagnosis. The patient is facing a chronic condition, with chronic treatment and of course their psychological mood changes. What they need to know is that if they follow their doctor’s instructions and are monitored whenever they need to be, then they need not be afraid of the severe progression of the disease and otherwise live a completely normal life without special restrictions.
Patients suffering from glaucoma should have a complete eye examination to measure their eye pressure and an ophthalmoscopy every 3-4 months by their doctor. They should also undergo a glaucoma study using all of the above technology every 6 months. These new technologies are supplementary and the purpose is to see if there is any further development of the disease over time in order to make the appropriate decisions.
Although patients with ocular hypertension do not have glaucoma and probably do not need chronic treatment they should be monitored the same as glaucoma patients, so that should the first lesions occur they can be kept in these early stages.
Prevention of glaucoma is very important. People with a family history of glaucoma should be screened once a year as a precaution by their ophthalmologist. Also, myopic patients, diabetics and patients with cardiovascular problems should be checked as a precaution once a year. Also, everyone should have had an eye check-up at least once in their life by the age of 40. After this age it is good to have a check-up by their ophthalmologist once every 1-2 years. We remind you that glaucoma has no symptoms and that most cases are diagnosed by chance.
Also, when glaucoma patients go to their ophthalmologist they should be more concerned about the health of their optic nerve and less about the pressure in their eyes. So, never forget to ask: How is my optic nerve this time, doctor?
How is glaucoma treated?
The aim of treatment in glaucoma patients is to avoid worsening of the damage to the optic nerve, optic fibres and visual field. The main treatment for glaucoma is to maintain low intraocular pressure. Drug technology offers many eye drops capable of achieving this goal. Glaucoma research focuses on finding drugs that will achieve increased blood flow to the optic nerve and therefore its better nutrition but also drugs that will mainly protect the optic nerve (neuroprotection). Today, there are already some such drugs and research is endeavouring to increase the weapons to fight glaucoma.
1. MEDICINES
 In the form of eye drops we can have one type or a combination of eye drops. The doctor decides which treatment is appropriate and if changes are needed. Some of the drugs achieve an increased blood flow to the optic nerve and some others neuroprotection. In special cases, pills may be given for a short time to reduce the eye pressure. Pills can be given for a longer period of time to increase blood flow to the optic nerve. The treatment is for life.
In the form of eye drops we can have one type or a combination of eye drops. The doctor decides which treatment is appropriate and if changes are needed. Some of the drugs achieve an increased blood flow to the optic nerve and some others neuroprotection. In special cases, pills may be given for a short time to reduce the eye pressure. Pills can be given for a longer period of time to increase blood flow to the optic nerve. The treatment is for life.
Treatment of simple ocular hypertension is not necessary if there are no lesions in the above tests and as long as the pressure does not exceed 25-26. But constant monitoring is required.
2. LASER
It is a safe and painless method that is indicated for certain types of glaucoma and is usually a supplement to medication.
Laser trabeculoplasty (photo 1) is done to facilitate the drainage of aqueous humour from the angle between the iris and the cornea. It is done with the help of a special lens and local anesthesia with drops. (Photo 2)
In some eyes that have an anatomical predisposition for acute glaucoma or eyes that have already suffered from acute glaucoma, laser iridotomy needs to be performed preventively. (Photo 3). This operation is also very simple, is done under local anesthesia, and does not require hospitalisation.

Φωτ. 1

Φωτ. 2

Φωτ. 3
3. SURGERY
Surgery is done if the two previous treatments fail, or even earlier if the doctor deems it appropriate. We usually intervene when drugs and laser do not regulate the eye pressure and when, despite the treatment, there is a worsening of the clinical condition. The surgery achieves the best drainage of eye fluid through an opening that is created.


The operation (trabeculectomy) is not intended to reverse the damage caused by glaucoma. This is irreversible. Neither is it intended to provide better vision but helps significantly to prevent further damage to the visual field and reduces intraocular pressure to levels that are considered low.
Prevention
The best treatment for a chronic disease such as glaucoma is prevention. Today everyone, especially if they belong to one of the high-risk groups mentioned earlier, must have an eye examination at least once a year after the age of 35-40. This allows early diagnosis and prevents the unpleasant future consequences of glaucoma, which unfortunately are still observed today. Screening (before symptoms are evident) for glaucoma is a quick and inexpensive screening test that targets the entire population and tries to identify which individuals have initial lesions or which are suspicious and need further investigation.
The glaucoma patient can live a normal life, as long as they follow the instructions and treatment recommended by their doctor as well as being checked frequently. Only with monitoring can we know the progression of the disease and how to deal with it.